Steak Dinners, Sales Reps and Risky Procedures: Inside the Big Business of Clogged Arteries
NEW: About one month ago, we received an anonymous tip:
— Annie Waldman (@AnnieWaldman) February 16, 2023
"PLEASE look into what happened at the Robert J Dole VA…hundreds of local military heroes had their legs mutilated…and nobody has been held accountable."
And so I started to dig….a thread:https://t.co/rvdTtkBiIU
On June 14, 2017, just before noon, a doctor made an incision near a patient’s groin. Kari Kirk, a representative for the world’s largest medical device company, Medtronic, looked on and began texting her colleague a play-by-play.
“Fixing both legs from the ankles,” she wrote.
It was a fairly common procedure at the Robert J. Dole Veterans Affairs Medical Center in Wichita, Kansas, performed to treat blockages in the leg vessels.
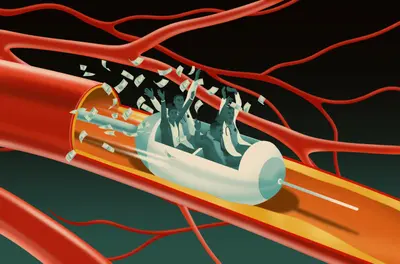
Within reach were an array of Medtronic products: tubes with blades attached to shave hardened deposits off of artery walls; stents to widen blood vessels; balloons coated with therapeutic drugs.
Each time a doctor puts a foreign device in someone’s body, it carries a risk of complication, which can include clots or even require amputation. So medical experts, research and even Medtronic’s own device instructions urge doctors to use as few as are necessary.
But, as revealed in Kirk’s text messages, this doctor took an aggressive approach.
“Just used 12 [drug-coated balloons]!!” Kirk texted her colleague.
“Does that mean I owe u $$,” he responded.
“Thats what I’m thinking!!! 🤣,” she said. “And now 14 balloons!😳”
“😜- but only one stent so far??”
“So far!”
As the texting continued, her colleague replied, “U are going to want to start going to the VA all the time.”
The messages, recently unsealed in an ongoing whistleblower lawsuit, give a window into the way money and medicine mingle in the booming business of peripheral artery disease, a condition that afflicts 6.5 million Americans over age 40 and is caused when fatty plaque builds up in arteries, blocking blood flow to the legs.
Representatives from companies are often present during vascular procedures to guide doctors on how to use their complex devices. This kind of access has the potential to influence treatment plans, as companies and their representatives profit when more of their product is used.
The suit, filed in 2017 by a sales representative for a competing medical device firm, alleges an illegal kickback scheme between Medtronic and hospital employees. According to the complaint and documents released in the suit, between 2011 and 2018, VA health care workers received steakhouse dinners, Apple electronics and NASCAR tickets, and in turn, Medtronic secured a lucrative contract with the hospital. Meanwhile, the company’s representatives allegedly “groomed and trained” physicians at the facility, who then deployed the company’s devices even when it was not medically indicated.
Independent from the whistleblower suit, internal investigators at the Wichita facility have also examined the treatment patterns of its vascular patients in recent years and found numerous cases where medical devices were used excessively. While it’s not uncommon to deploy several devices, a medical expert on the investigation team found that the VA doctors sometimes used more than 15 at a time — one used 33 — deviating from the standard of care.
“It is unconscionable — there can be no valid medically acceptable basis to cram so many devices into a human being,” wrote attorneys representing the whistleblower in legal filings from January 2023. “This is not medical treatment. This is abuse.”
Dr. Kim Hodgson, former president of the Society for Vascular Surgery and an expert retained by the plaintiff, said the findings of the internal review of patient data raise “a high level of concern regarding necessity of treatment provided,” according to case documents.
Medtronic declined to respond to ProPublica’s questions, citing the ongoing litigation. “These allegations are false and Medtronic is defending against these claims in court,” said Boua Xiong, a spokesperson for the company. Medtronic representative Kirk declined to respond to ProPublica’s request for comment.
The hospital investigation found that amputations increased sixfold in the same time frame as the procedures in question, according to internal emails, but made no conclusion about whether those two things were connected. ProPublica reached out to the VA to ask whether any patients had been harmed.
The VA is “conducting an extensive review of patient care” at the Kansas hospital, “including the number of devices used on patients — to make sure that Veterans were not harmed by any procedures,” press secretary Terrence Hayes said. So far, the VA’s investigation has found no “quality of care issues,” he said, and the investigation will continue “until every Veteran’s case has been reviewed.” (Read the full statement here.) Neither the department nor the hospital has taken formal action against the medical providers, Hayes said.
The medical group that had a contract with the VA for vascular interventions, Wichita Radiological Group, did not respond to ProPublica’s requests for comment, nor did the doctors named in the suit: Dr. Shaun Gonda, Dr. Bret Winblad and Dr. Kermit Rust. It is unclear from the case documents which doctors conducted which procedures. Eric Barth, an attorney for the medical group, denied the allegations in recent legal filings, calling the claims “baseless” and the lawsuit a “witch hunt.”
The lawsuit comes amid growing concern about one of these procedures — atherectomies — after researchers and doctors have uncovered patterns of excessive and inappropriate use. Recent research has found that this procedure, a common but costly treatment to shave or laser plaque from blood vessels, is not more effective than cheaper alternatives and may even be associated with a higher risk of complications including amputation. In recent years, several doctors and clinics have been investigated for allegedly takingadvantage of Medicare’s reimbursement rates, and one study found that many doctors are resorting to atherectomies in the earliest stages of peripheral artery disease, against best practices that urge noninvasive treatment.
“Atherectomy is important in certain settings. But it’s being used in a way that is entirely inappropriate and it’s largely driven by the incentive structure,” said Dr. Caitlin Hicks, the lead author of the study and an associate professor of surgery at Johns Hopkins University School of Medicine.
Although different payment structures govern the care of veterans, the whistleblower lawsuit alleges that outside physicians, paid hourly by the Dole VA, were motivated to conduct longer and more complex procedures that would earn them higher payment.
Under different circumstances, the patient in the procedure room on that summer day could have been done after two hours.
But, 150 minutes in, those Medtronic representatives were still texting. At that point, more than 15 of their vascular devices had been used, including stents, balloons and those for atherectomy.
“Long case!” Kirk’s colleague texted. “Is it looking ok??”
“It is,” she said. “Thought we were done a few times! Now he’s going back in to cut again!”
A little while later, she texted: “….17!”
He texted back: “😆😆😂😂”
Hospital leaders had been scrutinizing the use of these procedures at the Dole VA for years.
In 2017, shortly after Rick Ament was hired to lead the facility, he noticed something was amiss. While the longtime hospital administrator was poring over the finances, he was alarmed to discover that the relatively small Dole VA had one of the most expensive cardiac programs in the country. As Ament dug deeper, he realized vascular interventions were the reason.
“It just did not make sense that the acuity level of our patients would generate such extreme cost variances from the norm,” he testified in December, in a deposition for the whistleblower case. “It was so significant, we needed to get to the bottom of it.”
Ament, a second generation Air Force veteran, quietly assembled a task force to investigate why the facility had purchased so many medical devices for these procedures. After they examined inventory records, calculating the total number of medical devices and the cost of devices per patient, they grew concerned.
“We were more expensive than, I believe it was, the top 10 hospitals in the VA combined,” he said. “My feeling was that we either had very, very bad providers or we had product walking out the door.”
Ament enlisted experts from other VA hospitals to help his team investigate, including an administrative officer who could understand finances and a respected interventional radiologist who could examine records. The task force gathered a list of patients from 2016 to 2018, according to internal emails, and analyzed their medical charts.
According to internal VA documents released through the whistleblower suit, the review found a number of clinical failings: Evidence-based medicine had not been followed in the majority of cases reviewed. Procedures were over-aggressive, treating lesions that should have been left alone. And there was a total disregard for established best practices for treating peripheral artery disease.
One of the experts on the investigative team explained to Ament that while it was not uncommon for doctors to use a couple of devices in one intervention, the total number of devices in many of the procedures at his facility went into the double digits, sometimes five times the expected amount.
In one encounter, a doctor deployed 33 devices in one procedure — three atherectomy devices, nine stents and 21 balloons.
This use of devices was exorbitant, Ament came to understand. “I want to say the term ‘egregious’ was used,” he testified. “It was kind of like validation, but I really wish I was wrong.”
“Did it make you concerned for patient care?” a lawyer asked during the deposition.
“It did,” Ament replied.
A member of his task force pulled data for veterans who had leg amputations due to vascular disease. Over five years, the number of veterans who had amputations increased, from about six in 2013 to 38 in 2018, according to internal emails released in the suit. The VA did not respond to ProPublica’s questions about the rise in amputations or whether it was due to complications from the procedures.
Even though Ament testified in December 2022 that he became aware of the excessive use of devices during his investigation that began about five years ago, neither he nor the VA have publicly acknowledged these findings outside of the lawsuit. It is unclear whether VA representatives informed the patients whose records were reviewed about their findings. ProPublica reached out to more than half a dozen veteran community groups in the Wichita area and none were aware of the investigation nor the allegations of overuse of vascular procedures at the facility.
The VA says that if its ongoing review finds instances of substandard care, it will reach out to affected patients and inform them about possible complications and benefits they may be entitled to. The press secretary said the review will take several months. Ament declined to respond to ProPublica’s questions, citing the ongoing case.
In 2018, Ament turned over his findings to the criminal division of the VA’s Office of Inspector General. He also shut down interventional radiology procedures at the facility’s catheter lab.
Federal agents separately opened an investigation into the same unit in the facility, looking into allegations of kickbacks.
More than 40 pages of expense reports from Medtronic, revealed in the whistleblower case, show sales representatives treating Dole health care workers to hundreds of meals over several years — lunches at Dempsey’s Biscuit Co.; business meals at the Scotch & Sirloin steakhouse; dinner at Chester’s Chophouse & Wine Bar, price per attendee: $122.39.
Federal agents obtained the receipts.
“Robert J. Dole VAMC employees may have received improper gratuities, in the forms of paid lunches, dinners, etc., from sales representatives from Medtronic,” wrote Nathen Howard, a special agent in the VA OIG, in an investigation memo from February 2019.
This kind of relationship could violate VA policy, which forbids federal employees from receiving any gifts, including meals, from people who do business or seek to do business with a federal institution. For health care workers, violating this policy could have serious implications for patients. Numerous studies have shown that even modest industry-sponsored gifts, including meals, may influence prescribing or treatment behavior of health care professionals.
The agents opened their investigation into kickbacks at the Wichita facility in response to the whistleblower lawsuit, which was filed by Thomas Schroeder in 2017. The VA OIG would not confirm or deny whether it was continuing to investigate kickbacks at the facility. The VA did not directly answer ProPublica’s questions about kickbacks at the Dole VA, but it said that every employee must complete an annual ethics training, which covers gift rules.
In recent years, Medtronic has settled a handful of other cases that have alleged kickbacks between company representatives and health care professionals.
In 2018, Medtronic’s subsidiary Covidien paid $13 million to settle claims with the U.S. Department of Justice that it paid kickbacks to health care institutions that used its mechanical blood clot devices. In 2019, the same subsidiary paid $17 million to resolve allegations that it provided in-kind marketing support to doctors using its vein products. And in 2020, Medtronic paid more than $8 million to settle claims that representatives had paid kickbacks to a neurosurgeon, including scores of lavish meals at a restaurant that the doctor owned, to induce him to purchase the company’s medication pumps.
Schroeder’s lawsuit is not the first time Medtronic’s vascular devices were named in an alleged kickback scheme. In early 2015, Medtronic acquired Covidien, and shortly after the merger, its subsidiary ev3 Inc.agreed to pay $1.25 million to resolve allegations that it had paid doctors who were “high volume users” of its atherectomy devices to act as evangelists for the company, and had provided physicians with company shares to participate in clinical trials for their tools.
The whistleblower in this earlier case, a former sales representative for the company, also alleged that the subsidiary was gaming Medicare’s payment system. Hospitals were often hesitant to conduct atherectomy procedures because of the low reimbursement rates. According to the suit, sales representatives encouraged doctors to admit patients for longer stays to reap greater reimbursements and make a profit, even though such stays were often not medically indicated.
“Medical device makers that try to boost their profits by causing patients to be admitted for unnecessary and expensive inpatient hospital stays will be held accountable,” special agent Thomas O’Donnell, from the Office of Inspector General at the U.S. Department of Health and Human Services, said in a press release for the settlement. “Both patients and taxpayers deserve to have medical decisions made based on what is medically appropriate.”
Medtronic spokesperson Xiong said that in each case, the company “cooperated fully with the DOJ to resolve its concerns and, where wrongdoing was found, took appropriate remedial action.”
Seton Hall Law School professor Jacob Elberg, a former assistant U.S. attorney for the District of New Jersey who led its health care and government fraud unit, is concerned by the frequency of such settlements in the last two decades. “There are, at this point, real questions as to whether the sanctions imposed by DOJ are sufficient to deter wrongdoing and to lead to meaningful change, especially within the medical device industry.”
Although the Department of Justice has declined to intervene in the lawsuit involving the Dole VA at this time, the case is ongoing and further depositions with Medtronic sales representatives and a former VA employee are scheduled for this month.
VA employees and doctors named in the suit declined to comment or did not respond to ProPublica’s questions about the alleged kickbacks and whether sales representatives may have influenced veterans’ treatment plans. In interviews with federal investigators, according to released transcripts, several of the employees who were questioned denied receiving frequent meals from sales representatives, contradicting Medtronic’s expense reports.
Their statements also stand in contrast to Medtronic representative Kari Kirk’s final text messages during that procedure in June 2017, which ultimately lasted more than three hours.
“Now u done??” her colleague asked.
“Just finished,” she texted. “Running to get them lunch!”
“👍🍺🎉”
by Annie Waldman ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.