Sleep aids are common solution for those suffering from insomnia and are often recommended by doctors for those experiencing mild insomnia. They’re available at every pharmacy and are usually pretty cheap. They coax the body into a drowsy state and lead you to fall asleep. Unlike narcotic sleeping pills they don’t “knock you out” for a predetermined time.
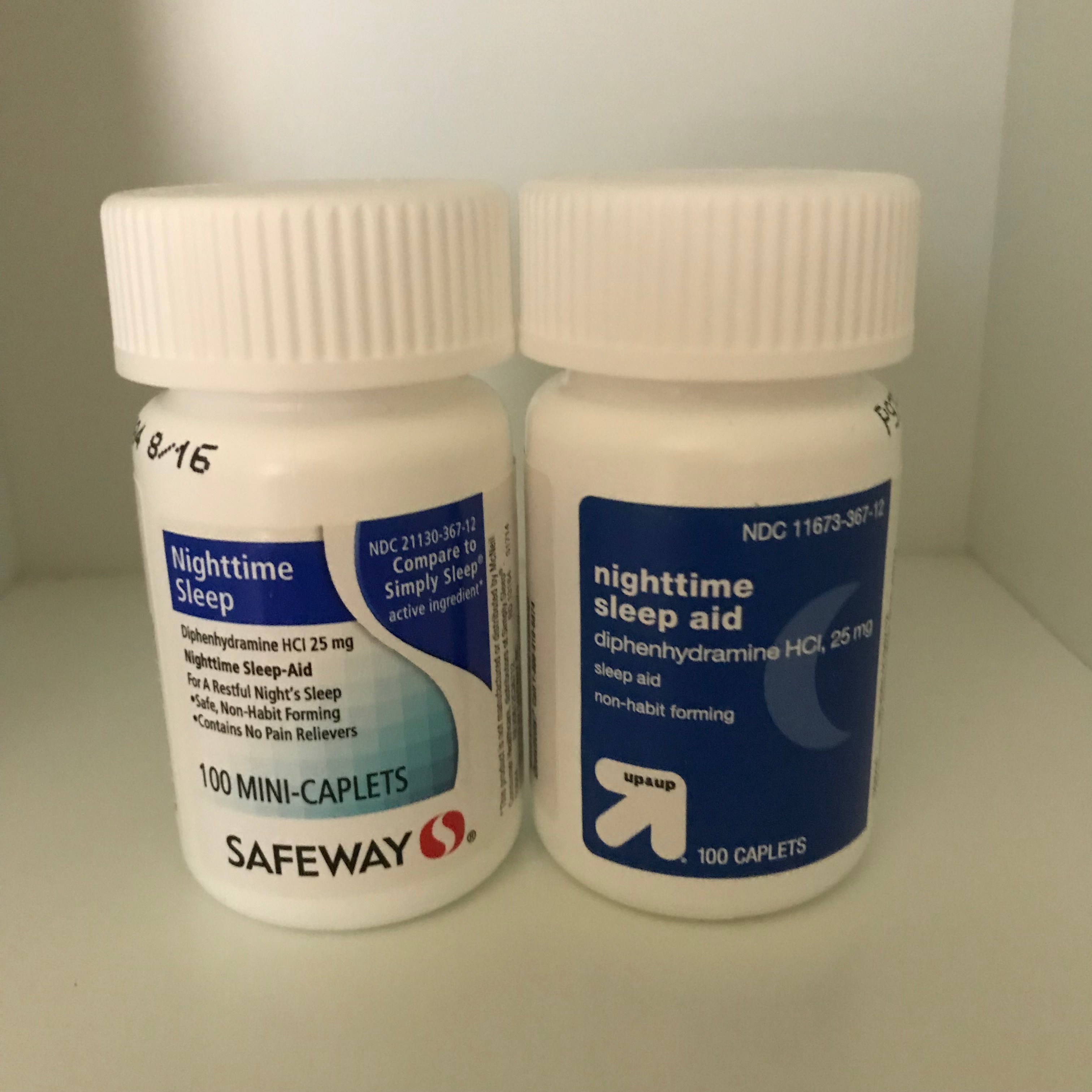
These sleep aids are just antihistamines, the same drugs used to fight colds and allergies. Many people have experienced success with these sleeping aids. They make you drowsy and get you over that initial hump so you can get to sleep.
But others find that these sleeping aids aren’t the cure-all they’re made out to be. If you don’t get eight hours sleep, you might wake up and find yourself more tired than you otherwise would have been. They can lead to disruptive morning drowsiness and headaches.
Sleeping pills contain the usual side effects – constipation, diarrhea, heartburn, weakness. But doctors also warn about a more insidious set of consequences, called parasomnias. These are behaviors that occur when you’re asleep over which you have no control. The most common parasomnia is sleepwalking, but others include sleep eating, having sex while asleep, and even sleep driving. Parasomnias are very difficult to detect. The likelihood of experiencing parasomnias is increased by sleeping pills.
Long-term effects of antihistamines
If you’ve been using products containing antihistamines (Benadryl, Simply Sleep) continuously for years, you might want to switch out to a “natural” remedy like melatonin and save the sleep aid for occasional use. Because melatonin is contra-indicated with some medications, check with your healthcare provider first.
A study from the University of Washington links long-term use of common medications — including over-the-counter drugs for insomnia and hay fever — to a higher risk of dementia, including Alzheimer’s disease. Medications in the study included antihistamines found in Benadryl and sleep aids found in Tylenol PM. The researchers tracked 3,500 older adults for use of medications with an anticholinergic blocking effect on the nervous system. Medications that act on the brain this way are known to cause short-term problems with cognition and thinking. Think: don’t drive or operate heavy machinery, but now researchers believe there’s a long-term effect as well. The problem is, there are hundreds of drugs with anticholinergic properties, including antacids,
- Amitriptyline (Elavil)
- Atropine
- Chlorpheniramine (Actifed, Allergy & Congestion Relief, Chlor-Trimeton, Codeprex, Efidac-24 Chlorpheniramine, etc.)
- Desipramine (Norpramin)
- Dicyclomine (Bentyl)
- Diphenhydramine (Advil PM, Aleve PM, Bayer PM, Benadryl, Excedrin PM, Nytol, Simply Sleep, Sominex, Tylenol PM, Unisom, etc.)
- Doxepin (Adapin, Silenor, Sinequan)
- Hydroxyzine (Atarax, Vistaril)
- Hyoscyamine (Anaspaz, Levbid, Levsin, Levsinex, NuLev)
- Imipramine (Tofranil)
- Meclizine (Antivert, Bonine)
- Nortriptyline (Pamelor)
- Olanzapine (Zyprexa)
- Oxybutynin (Ditropan, Oxytrol)
- Paroxetine (Brisdelle, Paxil)
- Prochlorperazine (Compazine)
- Promethazine (Phenergan)
- Pseudoephedrine HCl/Triprolidine HCl (Aprodine)
- Scopolamine (Transderm Scop)
- Tolterodine (Detrol)
 The Squirrel says: Instead of using these drugs, ask your doctor about Celexa and Prozac for depression, and second-generation allegory remedies like Loratadine (Claratin), Fexofenadine (Allegra) and cetirizine (Zyrtec), which are antihistamines without anti-cholinergic effects. Make sure you take the lowest dose for the least amount of time needed to alleviate symptoms. And don’t stop any prescribed therapy without consulting your doctor.
The Squirrel says: Instead of using these drugs, ask your doctor about Celexa and Prozac for depression, and second-generation allegory remedies like Loratadine (Claratin), Fexofenadine (Allegra) and cetirizine (Zyrtec), which are antihistamines without anti-cholinergic effects. Make sure you take the lowest dose for the least amount of time needed to alleviate symptoms. And don’t stop any prescribed therapy without consulting your doctor.
Finally, if you do decide to take a sleeping pill, you really shouldn’t wash it down with alcohol no matter how great the temptation.